In the labyrinth of human health, few paths are as winding and arduous as the journey to wound healing. Venous ulcers, those persistent and often painful lesions that bloom on the legs, are a particularly vexing challenge. They form when veins in the lower limbs struggle to send blood back to the heart, causing a cascade of complications that culminate in these stubborn sores. Despite their prevalence and the discomfort they bring, venous ulcers remain an enigma to many, shrouded in medical jargon and misconceptions.
In this article, we will unravel the mystery of venous ulcers, delving into the intricate dance of circulatory dynamics that spark their genesis. We will explore the myriad of treatment options available, from time-honored compression therapy to cutting-edge advancements in wound care. Whether you are a patient seeking solace, a caregiver looking for guidance, or a healthcare professional wanting to broaden your understanding, join us as we map out the landscape of venous ulcer care. Let’s uncover the pathways to healing and the hope that lies within.
Understanding Venous Ulcers: Causes and Risk Factors
Venous ulcers arise when veins in the legs fail to send blood back to the heart efficiently, causing a condition known as chronic venous insufficiency. As a result, pressure builds up within the venous system, leading to skin breakdown and the formation of ulcers. This condition is often marked by swollen, achy legs and a heavy feeling, particularly after extended periods of standing or sitting.
Several factors increase the susceptibility to venous ulcers. Risk factors include:
- Age: Older adults are more prone to developing venous insufficiency.
- Gender: Women are generally at higher risk due to hormonal differences and pregnancy.
- Family History: Genetics play a significant role in venous health.
- Obesity: Excess weight adds pressure on the veins, complicating blood circulation.
- Physical Inactivity: Prolonged inactivity can weaken the leg muscles and exacerbate venous problems.
For a more detailed understanding, consider the relationship between chronic conditions and venous ulcers. Chronic diseases like diabetes and hypertension also impair vascular health, making them contributing factors. For example, high blood pressure intensifies vein pressure, while diabetes can lead to nerve damage that might obscure early symptoms.
| Risk Factor | Description |
|---|---|
| Age | Older age increases the risk |
| Gender | Women have a higher propensity |
| Family History | Genetic predisposition matters |
| Obesity | Excess weight increases vein pressure |
| Inactivity | Weakens leg muscles over time |

Early Detection: Identifying the Signs and Symptoms
Venous ulcers can be insidious, often developing slowly and presenting subtle signs initially. Recognizing these early indicators is crucial for timely intervention. The skin around the ankle or calf may gradually become discolored, usually taking on a reddish or purplish hue. This may be accompanied by itching and a sensation of heaviness in the leg.
It’s not uncommon for the affected area to feel hard or tight, alongside noticeable swelling that worsens throughout the day but improves with elevation. The skin may feel warm to the touch, and in some cases, small, shiny patches can appear as the condition progresses. These changes can be mistakenly dismissed as minor irritations or symptoms of other conditions, making vigilance essential.
If venous ulcers advance without appropriate care, more telling symptoms emerge. These include persistent pain, open sores that are slow to heal, and wound drainage. The pain may initially seem moderate but can become severe, particularly if the ulcer gets infected. Monitoring these signs ensures early treatment, which significantly improves outcomes.
To facilitate easy identification, here’s a quick reference guide:
| Symptom | Description |
|---|---|
| Discoloration | Reddish or purplish skin |
| Itching | Persistent and around the ulcer site |
| Swelling | Increases during the day, reduces with elevation |
| Soreness | Open, slow-healing sores with potential drainage |
Recognizing these early signs and symptoms empowers individuals to seek timely medical advice and implement preventive measures, thus mitigating the risks and complications associated with venous ulcers.
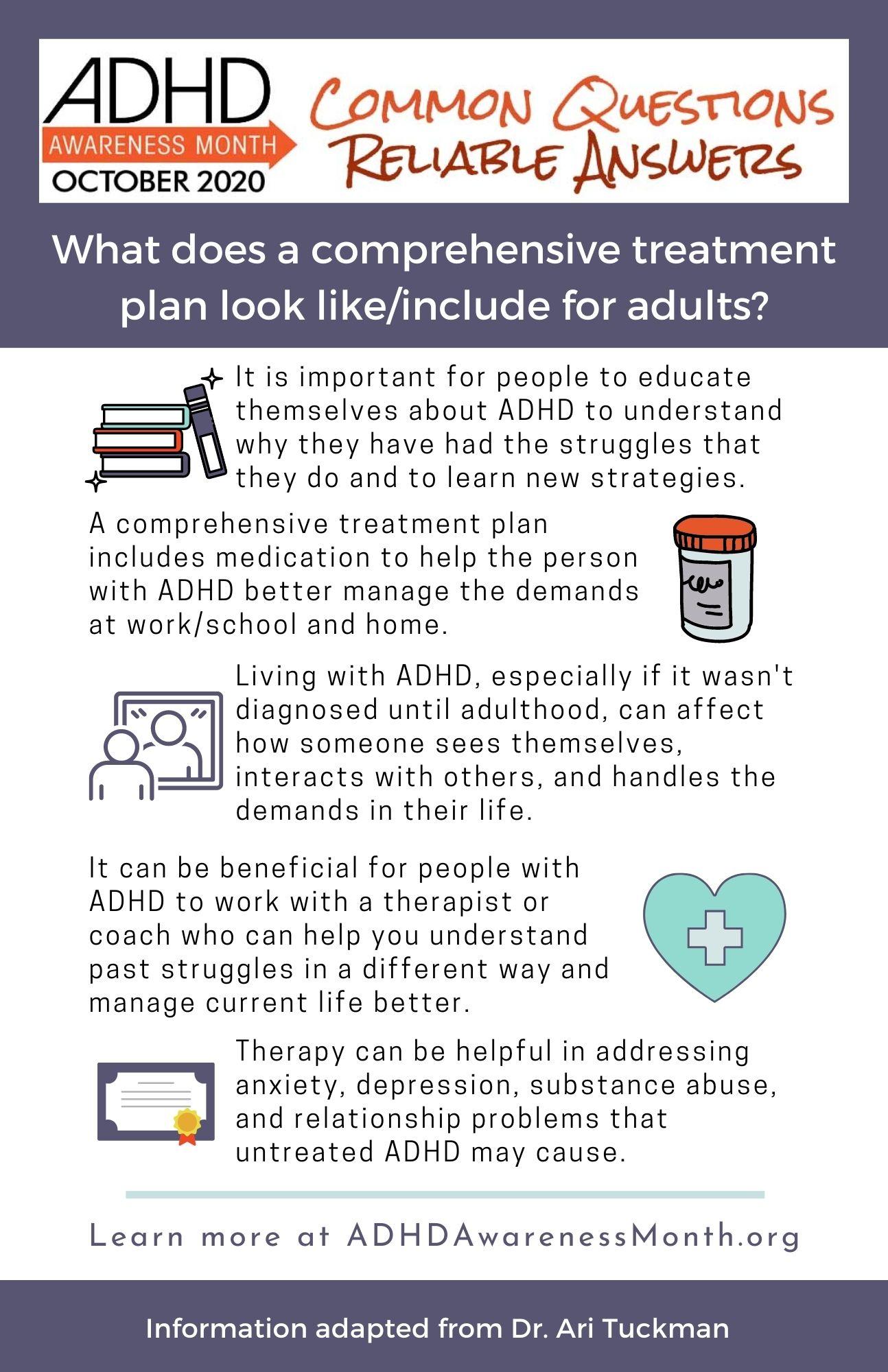
Comprehensive Treatment Plans: Medical and Home Care Strategies
Crafting a comprehensive treatment plan for venous ulcers is crucial in achieving optimal healing and minimizing recurrence. A combination of medical interventions and home care strategies ensures that the wound environment is conducive to healing while addressing the root causes of the condition. Medical professionals often initiate treatment by assessing the severity of the ulcer and determining the appropriate wound care regimen, which may include debridement, infection control, and specialized dressings.
Medical strategies often involve the implementation of compression therapy, a cornerstone of venous ulcer management. Compression stockings or bandages are used to enhance venous return, reduce edema, and promote wound healing. Additionally, medical-grade honey and advanced topical agents play a significant role in accelerating the healing process and fighting infections. For severe cases, more advanced treatments such as endovenous laser therapy or sclerotherapy may be necessary.
Home care practices are equally vital in promoting ulcer healing and preventing complications. Patients are advised to practice effective leg elevation to minimize swelling and enhance blood flow. Maintaining proper wound hygiene is imperative; this includes regular cleaning, appropriate dressing changes, and monitoring for signs of infection. Lifestyle changes such as weight management, increased physical activity, and smoking cessation further support the overall treatment plan.
| Home Care Tips | Details |
| Compression Use | Wear as prescribed, remove at night. |
| Leg Elevation | Raise legs above heart level for 30 minutes, 3-4 times daily. |
| Footwear | Opt for comfortable, supportive shoes. |
| Diet | Balance diet with fruits, vegetables, lean proteins. |
Supporting home care with regular follow-up appointments ensures that any arising complications are promptly addressed. Collaboration between patients and healthcare providers fosters an understanding of disease management, encouraging adherence to treatment protocols. By integrating both medical and home care strategies, a holistic approach for venous ulcer care is achieved, promoting effective and lasting wound healing.

Advanced Therapeutic Options: Dressings, Compression, and Beyond
Healing venous ulcers requires a multifaceted approach to address both the symptoms and underlying causes. Advanced therapeutic options have evolved, providing better outcomes for patients and easing the burden on healthcare providers. At the forefront of these therapies are specialized dressings and compression techniques, supplemented by innovative adjuncts that go beyond traditional methods.
Dressings: The choice of dressing can significantly impact the healing of venous ulcers. Modern dressings offer a range of functions, including moisture management, infection control, and support for autolytic debridement. Popular categories include:
- Hydrocolloids: These dressings maintain a moist environment which promotes new tissue growth.
- Alginate Dressings: Derived from seaweed, they are excellent at absorbing exudate and maintaining a balanced moisture level.
- Antimicrobial Dressings: Infused with agents like silver or iodine, they help control infection, a common complication in chronic ulcers.
Compression: Compression therapy is a cornerstone in venous ulcer treatment as it improves venous return and reduces edema. Options range from elastic bandages to more advanced compression stockings and multi-layer systems designed to provide graduated pressure. An appropriately applied compression bandage can significantly hasten healing times by improving blood flow and reducing inflammatory response.
| Compression Type | Benefits |
|---|---|
| Elastic Bandages | Cost-effective, immediate application |
| Compression Stockings | Variety of pressures, durable for daily use |
| Multi-layer Systems | Enhanced support, consistent pressure |
Apart from dressings and compression, therapeutic interventions now also include advanced adjuncts like negative pressure wound therapy (NPWT) and growth factor treatments. NPWT involves applying a vacuum dressing to promote healing by reducing swelling and removing exudates. Similarly, growth factor treatments deliver essential proteins directly to the wound site, accelerating tissue regeneration and improving healing outcomes.
Preventive Measures: Lifestyle Changes and Long-Term Care Tips
Adopting healthy lifestyle changes is crucial in the management and prevention of venous ulcers. Regular physical activity is essential as it promotes circulation and reduces pressure on veins. Opt for exercises that focus on leg strength and flexibility, such as walking, swimming, or cycling. Additionally, consider integrating stretches into your daily routine, as they help maintain blood flow and prevent stiffness.
<ul>
<li><strong>Daily walks:</strong> Aim for at least 30 minutes.</li>
<li><strong>Stretching exercises:</strong> Perform leg stretches twice a day.</li>
<li><strong>Low-impact activities:</strong> Swimming and cycling are excellent choices.</li>
</ul>
A balanced diet plays a significant role in venous health. Ensure your meals are rich in vitamins C and E, zinc, and proteins, which aid in tissue repair and immune function. Keeping a healthy weight can also reduce the strain on your veins, lessening the likelihood of ulcer formation. To assist, focus on consuming plenty of fruits, vegetables, lean proteins, and whole grains while limiting processed foods and sugars.
<table class="wp-block-table">
<thead>
<tr>
<th>Nutrient</th>
<th>Sources</th>
</tr>
</thead>
<tbody>
<tr>
<td>Vitamin C</td>
<td>Citrus fruits, bell peppers, broccoli</td>
</tr>
<tr>
<td>Vitamin E</td>
<td>Nuts, seeds, spinach</td>
</tr>
<tr>
<td>Zinc</td>
<td>Meat, shellfish, legumes</td>
</tr>
<tr>
<td>Proteins</td>
<td>Lean meats, tofu, lentils</td>
</tr>
</tbody>
</table>
Compression therapy is another pivotal aspect of long-term care for venous ulcers. This technique helps improve blood flow in the legs, supports vein function, and can significantly reduce swelling. Compression stockings or bandages should be worn consistently, especially during the day when you are most active. Consult with your healthcare provider for a proper fitting to ensure maximum effectiveness and comfort.
maintaining good skin care around the ulcer site is vital. Keep your skin moisturized to prevent dryness and irritation, which can exacerbate ulceration. Use mild, fragrance-free lotions and soaps. Additionally, elevate your legs whenever possible to reduce swelling and promote healing. Simple tips like these can make a significant difference in your journey toward recovery.
Q&A
### Q&A: Healing Wounds: Venous Ulcer Care and Treatment Options
Q: What are venous ulcers and what causes them?
A: Venous ulcers are open sores that commonly occur on the legs. They are primarily caused by poor blood circulation, specifically venous insufficiency, where the veins in the legs are unable to return blood back to the heart efficiently. This condition often results in increased pressure in the veins, leading to the breakdown of skin tissue and the formation of ulcers.
Q: How can one identify if they have a venous ulcer?
A: Venous ulcers usually present as shallow, irregularly shaped open sores with a red base, often surrounded by discolored or hardened skin. They are typically located just above the ankle. Symptoms can include swelling, aching, and a heavy feeling in the legs, as well as itching or burning sensations around the ulcer.
Q: What are the primary treatment options for venous ulcers?
A: The main treatment options for venous ulcers focus on improving blood flow and promoting healing of the ulcer. These include:
-
Compression Therapy: Using compression stockings or bandages to help improve blood circulation in the legs.
-
Wound Care: Regular cleaning and dressing of the ulcer, utilizing various wound care products to maintain a moist healing environment.
-
Medications: Sometimes antibiotics are prescribed if there’s an infection, while other medications can help to address underlying venous issues.
-
Surgery: In some cases, surgical options such as vein ablation or vein stripping may be necessary to improve blood flow.
Q: Can lifestyle changes play a role in preventing and managing venous ulcers?
A: Absolutely. Lifestyle modifications are crucial for both preventing and managing venous ulcers. These include:
- Exercise: Regular physical activity can improve circulation and help in maintaining a healthy weight, which reduces pressure on the veins.
- Diet: A balanced diet rich in fruits, vegetables, and lean proteins supports overall health and healing.
- Leg Elevation: Elevating the legs above heart level can reduce venous pressure and swelling.
- Avoiding Prolonged Sitting or Standing: Regular movement is essential for good circulation.
Q: Is professional medical advice necessary for venous ulcer treatment?
A: Yes, professional medical advice is vital for diagnosing and treating venous ulcers properly. A healthcare provider can offer tailored treatment plans, monitor healing progress, and provide guidance on preventive measures. Ignoring professional advice can lead to complications, such as infections or more severe chronic conditions.
Q: Are there any emerging treatments or technologies for venous ulcers that show promise?
A: Emerging treatments like bioengineered skin substitutes, stem cell therapy, and growth factor treatments are showing promise in accelerating wound healing and improving outcomes for venous ulcer patients. Additionally, advances in diagnostic tools and minimally invasive surgical techniques are enhancing the ability to treat the underlying venous insufficiency more effectively.
Q: What is the prognosis for individuals with venous ulcers?
A: With proper treatment and lifestyle adjustments, many individuals can successfully heal from venous ulcers, though the process can be slow and requires consistent care. Recurrence is common, so preventive strategies and ongoing management are important to reduce the risk of future ulcers.
Q: Are there any support resources available for individuals managing venous ulcers?
A: Yes, there are various support resources available, including patient support groups, online forums, educational materials from healthcare providers, and specialized wound care clinics. These resources can offer emotional support, practical advice, and the latest information on treatment options.
By understanding the causes, treatment options, and preventive measures for venous ulcers, individuals can take proactive steps towards effective management and improved quality of life.
To Wrap It Up
As we close the pages on the intricate journey of venous ulcer care and treatment, it’s clear that healing wounds—both seen and unseen—requires a symphony of knowledge, compassion, and innovation. From time-tested compression therapy to the promising frontiers of regenerative medicine, the pathways to recovery echo the resilience of the human spirit. As we navigate the ever-evolving landscape of medical advancements, let us continue to blend science with empathy, ensuring that each step forward not only mends the physical but also uplifts the soul. With every bandage we unfurl and every solution we explore, we come closer to a future where healing is not just a hope, but a harmonious reality.






