In the often-invisible world of medical procedures, the seemingly mundane act of hair removal stands as a silent guardian. Delicately removing tiny strands from the surgical path, this practice within ear surgeries has sparked considerable debate and investigation. Nestled at the crossroads of hygiene and necessity, the question emerges: How much influence does hair removal truly have on the prevalence of post-operative infections? This article dives beneath the surface, exploring the intricate dance between scalpels and sterilization, shedding light on a practice that might just be the unsung hero in the fight against ear surgery infections. Join us as we unravel the clinical, procedural, and scientific threads of this overlooked yet pivotal aspect of surgical success.
Preoperative Hair Removal: A Double-Edged Sword
Hair removal before ear surgery is standard practice aiming to reduce infection risks by eliminating hair that could harbor bacteria. However, recent studies have brought attention to the **complications** associated with this procedure. Hair removal can disrupt the integrity of the skin barrier, inadvertently increasing susceptibility to infections. This paradox often leaves both patients and surgeons pondering whether the benefits outweigh the potential risks.
One significant consideration is the method of hair removal. **Shaving**, for example, can cause micro-abrasions on the skin, providing an entry point for pathogens. In contrast, **clipping** hair close to the skin surface without breaking it seems to be a preferable alternative. Some studies even suggest that clipping is associated with lower infection rates compared to shaving. Here’s a quick comparison of the risks involved:
| Method | Risk Level |
|---|---|
| Shaving | Higher (due to skin abrasions) |
| Clipping | Lower (minimal skin damage) |
Another **controversial topic** is the timing of hair removal. Performing the procedure too early before surgery may allow bacteria to repopulate the area, while doing it immediately before surgery might not leave enough time for the skin to recover from any inadvertent trauma. Current guidelines suggest hair removal within **a few hours** before surgery to strike a balance between these two concerns.
Despite the prevalent practices, some experts argue for **no hair removal at all** unless absolutely necessary. They emphasize modern aseptic techniques, enhanced sterilization methods, and the use of **antibiotic prophylaxis** as more effective means to prevent infections. Therefore, the debate continues, with ongoing research striving to find the optimal approach that maximizes surgical outcomes while minimizing the risk of infections.
The Microbial Battlefield: Hair Follicles and Surgical Sites
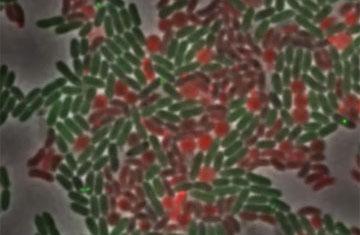
Hair follicles nestled deep within the skin are more than just cosmetic features; they are bustling micro-ecosystems where bacteria, fungi, and other microorganisms thrive. In the context of ear surgeries, these microbial inhabitants can turn into menacing foes. When surgeons prepare a patient, one common step is hair removal around the surgical site. This action, though seemingly straightforward, disrupts the delicate balance of microflora, potentially leading to unexpected consequences.
The practice of hair removal aims to reduce the risk of infection, but various studies suggest it can sometimes have the opposite effect. **Hair follicles**, once shaven or plucked, become exposed and irritated, opening the door for opportunistic pathogens. Post-operative infections can stem from these very openings. Key factors contributing to these infections include:
- **Types of hair removal techniques**: Shaving vs. depilatory creams
- **Microbial load**: Pre-existing bacteria vs. newly introduced pathogens
- **Post-operative care**: Proper wound management vs. negligence
Whether shaving or employing chemical depilatories, each method carries its own risk of skin irritation and infection. For instance, shaving with a razor can create micro-tears, leading to a higher chance of microbial invasion. On the other hand, depilatory creams, while less abrasive, can cause chemical burns in some individuals. To highlight these risks, consider the following comparison:
| Method | Risk Level | Common Issues |
|---|---|---|
| Shaving | High | Micro-tears, bleeding |
| Depilatory Cream | Moderate | Chemical burns, allergic reactions |
Ultimately, the decision on whether to remove hair prior to ear surgery should be meticulously weighed, considering the patient’s skin sensitivity and the surgeon’s expertise. Personalized strategies, rigorous sterilization protocols, and comprehensive post-operative care can collectively aid in minimizing infection risks, allowing patients to heal seamlessly and safely.

Techniques and Tools: Avoiding Inadvertent Harms in Hair Removal
Implementing proper techniques and using the right tools for hair removal can significantly reduce the risk of infections following ear surgery. **Precision** is key when dealing with the delicate area around the ears. Ensuring that the skin remains unbroken and intact minimizes entry points for pathogens. Here’s a snippet into the “do’s” and “don’ts” to maintain a sterile environment:
- Do: Use single-use, sterile razors.
- Don’t: Share razors, even among close family members.
- Do: Disinfect the area with an antiseptic before and after shaving.
- Don’t: Use old or dull blades that can cause micro-injuries to the skin.
Recommended Tools
Utilizing the correct tools can make a significant difference. Here’s a comparison of various hair removal methods:
| Method | Advantages | Disadvantages |
|---|---|---|
| Electric Trimmer | Quick, less skin contact | Requires thorough cleaning |
| Disposable Razor | Cheap, widely available | Requires proper disposal |
| Laser Hair Removal | Long-lasting | Expensive, needs professional oversight |
Beyond tools, the technique itself plays a significant role. **Dermatologists** recommend shaving in the direction of hair growth to avoid irritation and following up with a gentle, non-comedogenic moisturizer. Avoid pressing too hard on the razor, and always use a clean, sharp blade. Proper **aftercare** ensures that the skin barrier remains strong and resilient against potential infections.
Postoperative Outcomes: The Unseen Role of Hair Removal in Infection Rates
One often overlooked yet significant factor influencing the success of surgical procedures is the meticulous management of hair removal around the surgical site. In ear surgeries, this seemingly minor task can play a pivotal role in postoperative outcomes. Hair removal is not just about providing better visibility for surgeons; it serves a critical function in reducing the risk of infection, which can lead to severe complications.
**Key Benefits of Proper Hair Removal:**
- Minimized Risk of Bacterial Contamination
- Improved Wound Healing and Recovery
- Enhanced Adhesion of Surgical Dressings
Insightful studies reveal that the presence of hair can harbor bacteria, thereby increasing the likelihood of postoperative infections. This may explain why patients who undergo thorough hair removal experience fewer complications and faster recovery periods.
From a procedural standpoint, various hair removal techniques exist, each with its benefits and drawbacks:
| Method | Advantages | Disadvantages |
|---|---|---|
| Clipping | Quick, less skin irritation | May leave short stubble that traps bacteria |
| Shaving | Complete removal, enhanced visibility |
Skin abrasions, increased infection risk |
| Depilatory Creams | Non-abrasive, longer-lasting | Potential for allergic reactions |
**Factors Influencing Choice of Hair Removal Technique:**
- Patient’s Skin Sensitivity
- Location and Extent of Surgical Area
- Risk of Allergic Reactions
- Time Constraints
Surgeons must assess these factors meticulously to choose the most appropriate method, aiming to balance efficacy and safety. As advancements in medical protocols continue, the trend is towards minimizing skin trauma while maintaining hygiene.

A Surgeons Guide: Best Practices for Minimizing Surgical Infections
In modern surgical practices, the role of hair removal, especially around the ears, plays a crucial role in preventing post-operative infections. The area around the ear can be a hotspot for microbial activity due to natural oils and the complexity of ear anatomy. **Effective hair removal** can drastically cut down the microbial load, thereby significantly lowering infection risks associated with ear surgeries.
Several methods are commonly employed for hair removal, each with its respective pros and cons. These include:
- **Clipping**: Preferred by many surgeons due to its efficiency and safety profile.
- **Shaving**: Though effective, it can sometimes lead to minor skin abrasions, which could serve as entry points for bacteria.
- **Chemical depilation**: Less common but avoids the risk of cuts or abrasions. However, it may cause skin irritation in sensitive patients.
Maintaining proper protocols for hair removal is essential to ensure that the procedure itself does not become a source of infection. **Best practices** include:
- **Using sterile equipment**: Ensures that no additional pathogens are introduced during hair removal.
- **Timing the removal**: Performing it immediately before surgery to minimize the time bacteria have to colonize newly exposed skin.
- **Patient preparation**: Educating the patient about pre-surgical hygiene and ensuring they follow prescribed protocols.
A study comparing different hair removal methods and their impact on surgical site infections yielded interesting insights:
| Method | Infection Rate | Pros | Cons |
|---|---|---|---|
| Clipping | 2% | Fast, Safe | Short hair regrowth may cause itching |
| Shaving | 5% | Complete hair removal | Risk of abrasions |
| Chemical Depilation | 3% | No cuts or abrasions | Potential for skin irritation |
Q&A
Q&A: The Impact of Hair Removal on Ear Surgery Infections
Q1: What is the primary focus of the article about hair removal and ear surgery infections?
A1: The primary focus of the article is to explore the relationship between hair removal practices and the incidence of infections following ear surgery. It delves into how different methods of hair removal might affect the rate of post-operative infections and recovery outcomes for patients undergoing ear surgeries.
Q2: Why is hair removal considered an important aspect in ear surgery preparation?
A2: Hair removal is considered crucial in ear surgery preparation because the presence of hair can complicate surgical access, obscure the operating field, and potentially harbor bacteria that could lead to post-operative infections. By removing hair, surgeons aim to create a cleaner, more accessible surgical site, reducing the risk of contamination.
Q3: What methods of hair removal are commonly discussed in the context of ear surgery?
A3: The commonly discussed methods of hair removal in the context of ear surgery include shaving with a razor, using electric clippers, and employing depilatory creams. Each method has its pros and cons, and the article evaluates their impact on infection rates and overall patient outcomes.
Q4: How does shaving with a razor compare to using electric clippers in terms of infection risk?
A4: Shaving with a razor has been associated with a slightly higher risk of causing small nicks and abrasions on the skin, which can serve as entry points for bacteria and increase infection risk. In contrast, using electric clippers tends to be less invasive and gentler on the skin, potentially leading to a lower rate of post-operative infections.
Q5: Are there any studies or statistics mentioned in the article that support the findings?
A5: Yes, the article references several clinical studies and statistical analyses that compare infection rates among patients subjected to different hair removal techniques before ear surgery. These studies provide evidence that non-invasive methods like electric clipping are generally associated with lower infection rates compared to shaving with razors.
Q6: Does the article suggest any best practices for health professionals regarding hair removal in ear surgeries?
A6: The article suggests that health professionals should carefully consider the method of hair removal they use, favoring options that minimize skin trauma and reduce the risk of infection. It recommends comprehensive preoperative assessments and the use of electric clippers over razors when possible. Furthermore, it advises maintaining strict aseptic protocols during the hair removal process.
Q7: Are patient preferences or comfort discussed in the article?
A7: Yes, patient comfort and preferences are also discussed. The article highlights that some patients might have sensitivities or allergies to certain hair removal methods, such as depilatory creams. It encourages surgeons to take patient history into account and to communicate clearly about the hair removal process to ensure patient comfort and compliance.
Q8: What future research directions does the article propose?
A8: The article proposes future research directions focusing on long-term outcomes of different hair removal methods, including patient satisfaction, comfort, and the cost-effectiveness of various techniques. It also suggests exploring innovative hair removal technologies and their potential to further reduce infection risks in surgical settings.
Q9: How does the article conclude on the topic of hair removal and ear surgery infections?
A9: The article concludes by emphasizing the importance of choosing the right hair removal technique to minimize infection risks in ear surgeries. It underscores the need for continued research and adherence to best practices to enhance patient safety and surgical outcomes. The ultimate message is that meticulous preoperative preparation, including appropriate hair removal, plays a critical role in successful ear surgery interventions.
The Conclusion
As our exploration into the nuanced relationship between hair removal and ear surgery infections draws to a close, one thing is abundantly clear: the minutiae of pre-operative protocols can have profound implications. The gentle hum of a surgical razor may seem insignificant against the backdrop of advanced medical technology, yet its role in shaping patient outcomes is undeniably pivotal. By fostering a deeper understanding of this delicate interplay, both practitioners and patients are better equipped to make informed choices that safeguard well-being. the path to optimal health often winds through the smallest of considerations—a testament to the intricate tapestry of modern medicine.






